Smarter Medical Billing Starts Here
Automate what wastes time with our customized RCM services. Track what matters, and keep your revenue moving.


Because their global operations need accuracy, speed, and exceptional support.




Satisfied Providers
Customer Retention Rate
Revenue Improvement
Benefits That Matter. Features That Deliver.
We build solutions that work quietly in the background to solve real billing problems, handle workflows, and speed up claims.
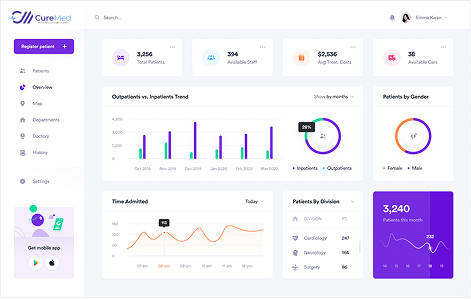
We handle every claim, every code, and every update, so you can focus on delivering care, not chasing payments. CureMed keeps your billing clean, compliant, and green.
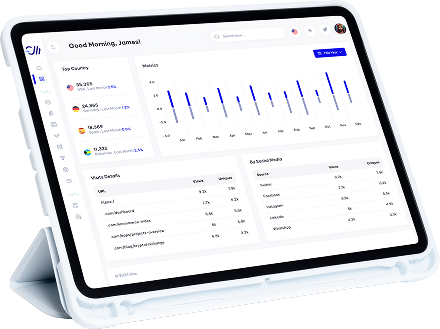
We dig deep into your billing data to find and plug cash leaks. CureMed’s medical billing audit services show you exactly how to improve your KPIs.
CureMed gives doctors and hospitals a complete software solution for medical billing and clearinghouse services with EHR integration. No multiple logins. No workflow gaps. Just complete control over your RCM from start to finish.
What We Do & Why It Works
CureMed’s services are built around a single cornerstone: making your billing smarter, faster, and easier to manage. We give doctors and hospitals the tools and support they need to get paid with confidence and clarity.
Services
We handle every submission, follow-up, and correction, so your claims go through clean and your revenue comes in fast.
View MoreBilling
We tailor billing to how each physician actually works, accounting for visit types, procedure mix, and the nuances of every payer.
View MoreManagement (RCM)
Streamline your entire revenue cycle to reduce administrative burden and improve operational efficiency.
View MoreAssistance
Our trained virtual assistants handle patient calls, scheduling, documentation, and follow-ups, keeping your operations and staff focused on care.
View MoreRecovery
We track, chase, and collect to accelerate your cash flow without straining your patient relationships.
View MoreServices
We handle licenses, board certifications, and payer enrollments, getting providers network-ready and revenue-ready from day one.
View MoreRun Your Practice Without The Paperweight
CureMed takes the weight of administration off your shoulders. Let us handle the work, so you can handle the healing. Our practice management services simplify the backend of your business with expert billing, automated workflows, and hands-on support that work as hard as you do. Maybe even harder.
Schedule Demo
We identify bottlenecks before they cost you, and then fix them with tools and talent that make your workflow smarter, not harder.
Forgo the stress and guesswork. Our built-in safeguards and real-time updates keep every process aligned with the latest payer and federal requirements.

Our Specialities
Leave the complexities of billing behind. We tailor every solution to your specialty, so you can focus on delivering care with confidence.
We decode neurological billing complexities to keep your reimbursements fast and accurate.
Your cardiac care drives outcomes. Our billing ensures it drives revenue, too.
Accurate billing for every joint and fracture. Your charts stay clear along with your revenue.
We support every delivery and exam with exact coding and care-focused revenue flow.
Every session. Every code. Count on smarter billing that reflects the full value of your psychiatric care.
Dialysis, transplant, and beyond, our billing systems are built for complex renal care.
From exams to procedures, your podiatry billing reflects the full value of foot and ankle care.
Code diabetes care, hormone therapy, and metabolic evaluations with flawless precision.
Have questions? We have answers. Our team’s just a click away.